What is conventional IVF?
In vitro fertilisation, or IVF, is a medical procedure used to help individuals who are struggling with infertility to conceive a child.
The process involves bringing together the eggs and sperm in the lab, where fertilisation can occur. The resulting embryos are then transferred into the uterus in the hopes of achieving a successful pregnancy.
What are the steps in the IVF process?
In a conventional cycle of IVF, the ovaries are stimulated with hormones to produce multiple eggs, which are then retrieved and fertilised with sperm in the lab. Once an egg has been fertilised with a sperm, an embryo is created.
This embryo is then allowed to grow in the lab for a number of days in a special incubator along with a culture solution that provides the necessary nutrients that mimic the natural environment before the embryo is then transferred into the uterus in the hopes of achieving a pregnancy.
If there are extra embryos that have not been transferred during a single cycle, you can opt to freeze any remaining suitable embryos for future use. For individuals who undergo fertility preservation, all suitable embryos that are created are frozen for future use.
The steps in more detail…
There are different protocols for conducting an IVF cycle and which one is the most appropriate will depend on an individual’s circumstances. However, the overall principles remain the same.
Step 1 – The stimulation phase
Initially, a course of daily injections is self-administered. These drugs stimulate the ovaries to produce a number of growing follicles (which are fluid-filled sacs within which the eggs reside) and also to control the ovulation so that these eggs are not released prior to them being collected.
The daily injections continue for a couple of weeks and this is known as the ‘stimulation phase’. During this phase, ultrasound scans are performed every few days looking at the ovaries and monitoring the uterine lining in order to monitor the progress of the growing follicles.
Blood tests might also be taken as required to check hormone levels. Once the follicles have grown sufficiently, and to a size where it is expected that a mature egg will be retrieved, a final ‘maturation injection’ is given, followed by the egg collection procedure two days later.
Step 2 – Egg and sperm collection
The collection procedure itself is carried out under anaesthetic - usually sedation, but sometimes local or general anaesthetic is used. Under ultrasound guidance, a needle is passed through the vaginal wall, then into the ovaries, and into each of the follicles. Fluid from within the follicles is drawn out and taken to the lab where an embryologist looks at this fluid under a microscope in order to retrieve the eggs.
At this point, we need sperm in order to fertilise the eggs that were retrieved. If the sperm is provided by a partner, we request them to produce a fresh sample around the same time as the egg collection is taking place. If the sperm has been previously frozen – for example, because it was surgically retrieved, due to chemotherapy treatment, or because the sperm is from a donor - then we unfreeze the stored sample.
The sperm, either fresh or frozen, is then prepared by the embryology team and assessed under the microscope. Ideally, only the moving, normal sperm is used and we discard any dead, abnormal, or non-moving ones.
Step 3 - Bringing the sperm and eggs together
When we have both the eggs and prepared sperm in the lab, the time comes to bring them together.
Depending on the sperm quality, we perform either conventional IVF insemination or intracytoplasmic sperm injection, also known as ICSI.
In conventional IVF insemination, roughly 100,000 swimming sperm are placed alongside each egg. This allows a degree of natural selection and relies on the sperm penetrating the cells surrounding the egg and fusing with it to achieve fertilisation.
ICSI involves using a microscope along with a tiny needle to inject a single sperm directly into each egg. Not all eggs will be of a high enough quality or mature enough to be suitable for injection. It’s also possible that some eggs may not survive the injection process itself.
The decision of whether to perform conventional IVF or ICSI is primarily dependent on the quality of the sperm, however, a number of other clinical factors are occasionally also taken into consideration.
Step 4 – Checking for fertilisation
The morning after the eggs and sperm have been put together, the embryology team checks to see if fertilisation has occurred overnight. Normal fertilisation occurs when there are two lots of genetic material, one lot from the egg and one from the sperm.
When there are three or more copies, or less than two, we consider that the egg has fertilized abnormally. This leads to abnormal embryo development and therefore we do not consider them suitable for embryo transfer or freezing.
Why might abnormal fertilisation occur?
There are many reasons why fertilisation may produce an abnormal embryo, and our embryologists may be able to explain further based on what type of abnormal fertilisation occurred.
Ultimately, fertilisation is a very complex biological process and while some of the steps and requirements are known, others are still poorly understood. In most cases, it is normal to observe some eggs that have not fertilised during an IVF or ICSI cycle.
On average 60-70% of eggs do achieve fertilisation, no matter how poor the sperm appear to be. Rarer is a low level or even complete failure of any of the eggs to fertilise. This can be caused by sperm factors, egg factors, or a combination of both.
However, when an egg and sperm do not fertilise, it is difficult to say with complete accuracy what the main reason is. Sometimes, even if the eggs and the sperm appear to be of very good quality, none of the eggs fertilise.
Low or no fertilisation after conventional IVF insemination happens in up to 5% of cases.
While failure of fertilisation after ICSI still occurs in up to 3% of cases. Although this might seem surprising, injecting the sperm inside the egg does not guarantee that the egg will fertilise.
The initial steps of fertilisation might be bypassed using ICSI but once the sperm is inside the egg, some important biological processes still need to take place.
Step 5 – Incubating the embryos
Once an egg has been successfully fertilised by a sperm, it has now become an embryo. We collect any embryos that have formed during IVF or ICSI and allow them to grow in the lab.
This is done within a specially controlled environment using state-of-the-art incubation systems to maintain the optimum temperature and oxygen levels, along with specially manufactured culture media, which provides all necessary nutrients. This is a process of constant optimisation with the ultimate aim of mimicking the natural environment within which a human embryo would normally develop.
Step 6 – Embryo transfer to the uterus
Over the next few days, the embryos are continuously evaluated and the best ones are selected for transfer into the uterus.
The number of embryos transferred depends on various factors, including the person’s age at the time of the egg collection and the quality of the embryos, however ideally, we would prefer and recommend transferring one good quality embryo at a time to avoid the risks associated with multiple pregnancy.
Any remaining embryos can be frozen for future use.
Step 7 – Testing for pregnancy
After the embryo transfer has been performed, we need to wait a couple of weeks before ascertaining if the embryo has successfully implanted and this is done through a pregnancy test.
Step 8 – Careful monitoring
If successful, the pregnancy will be monitored for any early pregnancy complications as required throughout the first few weeks. Once the pregnancy has successfully completed the first trimester, then antenatal care as per each individual’s local hospital protocol commences.
An important note – IVF success rates
IVF has a success rate that varies depending on the person’s age at the time of egg collection, the quality of the eggs and sperm, any other associated medical conditions, and a host of other factors. Therefore, headline figures of success can be misleading and each case needs to be individualised to their unique circumstances.
Our IVF success rates
With more than 35 years’ experience, we’ve delivered more than 5,300 babies. Being a leader in research enables us to provide the best possible clinical outcomes for all our IVF patients.
IVF Success rates
With more than 35 years’ experience we’ve delivered more than 5,300 babies. Being a leader in research enables us to provide the best possible clinical outcomes for all our IVF patients.
View our success rates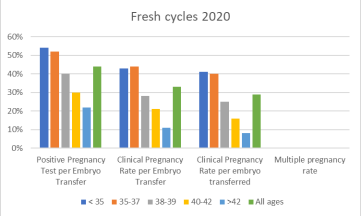
What our patients say
K
D
H & A
IVF costs from £3,995 plus medication
The cost of IVF treatment will depend on your circumstances. During your first consultation our fertility experts will work with you to outline a tailored treatment plan.
We are committed to ensuring our services are priced fairly and transparently, with no hidden costs involved.
Please click here to see pricing guideRisk of IVF
Fertility treatment is generally very safe and most who have it experience no problems with their health or pregnancy. However, there are some risks to be aware of, which include:
- Having a multiple pregnancy or birth (twins, triplets or more)
- Ovarian hyperstimulation syndrome (a severe reaction to fertility drugs)
- Having an ectopic pregnancy
- Possible birth defects (these are rare and research is still ongoing)
Want to know more about IVF Treatment
Contact our IVF team on 020 3957 7950 or via email on [email protected] to request more information about our IVF treatments.
